An IVF embryo grading chart answers the many questions that patients frequently ask their doctors about the different kinds of embryos and their likelihood for implantation. What is an embryo grading chart? How does it determine whether an embryo is considered good, fair, or poor?
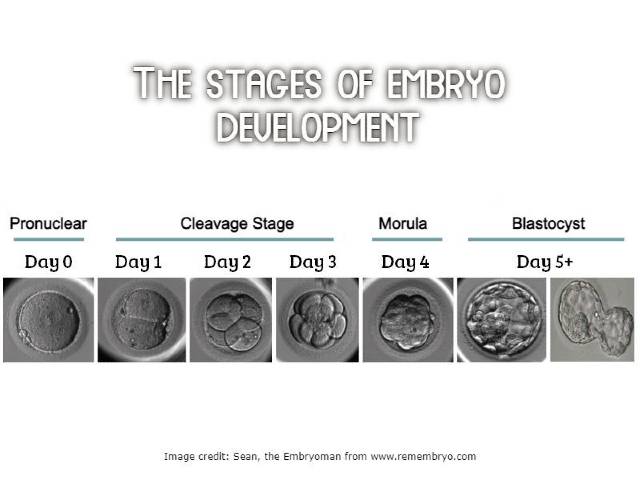
An embryo grading chart used in the IVF procedure to evaluate the quality of embryos across their various developmental stages.
An embryologist studies lab-created embryos under a microscope and grades them based on appearance during the in vitro fertilization process.
To maximize the likelihood of a successful pregnancy, embryologists and fertility doctors use the grading system to help them choose the most viable embryos for uterine transfer.
Embryo grading usually requires evaluating different characteristics of the embryo as:
- Cell number: The embryo’s cell count is determined. Ideally, at particular stages of development, embryos should attain a given number of cells.
- Symmetry: The symmetry and homogeneity of the cells are evaluated and a high degree of symmetry is a good sign.
- Fragmentation: The presence of tiny, asymmetrical cell fragments in the embryo. Higher-quality embryos have fewer fragments.
- Blastomere equality: This checks if the cells are equally divided
- Blastocyst formation (if applicable): At a later developmental stage, when the embryo forms a blastocyst, assessment of the inner cell mass (ICM) and trophectoderm (TE) may be part of the grading process.
The embryo’s appearance under a microscope is the only factor used to determine this grade. Although it provides a reasonable indication of which embryos have a better chance of surviving, the lack of information regarding the embryo’s genetic makeup keeps it from providing solid proof that the embryo is of the ‘baby-making’ sort.
Understanding the embryo grading chart will allow you to learn more about the quality of your embryos and your chances of success with IVF, unless you are planning for pre-implantation genetic testing of your embryos.
Day 3 embryo grading
Embryos at day 3 are also known as ‘cleavage stage’ embryos as the cells within them are dividing (cleaving) as the genetic material within them replicates, but the embryo at this stage is not growing.
Sometimes, while diving, a small portion of the cell’s cytoplasm separates and remains as an individual fragment inside the embryo. These fragments of cytoplasm do not contain nuclei but only the lost cytoplasm. While not much is understood about the causes of fragmentation, the embryos with too many fragments are considered poor because their cells have lost too much mass to be healthy.
Embryo grading at day 3 is done on the following three criteria:
- The number of cells in the embryo: A good-quality, normally-growing, embryo on day 3 would typically have 6-10 cells held within an outer shell called the Zona Pellucida (ZP). Research (1) shows that embryos with 8 cells or more are most likely to develop into a healthy blastocyst. Different clinics grade embryos upto 4 or 5 points, with 5 being the lowest.
- Fragmentation: Embryos with no or little fragmentation are labeled grade A, those with more than 10% fragmentation are grade B, and the ones with more than 25% and 50% fragmentation are labeled C and D grade respectively. Embryos with grade A and B are considered good and most likely to result in a healthy pregnancy.
- The appearance of cells under a microscope: Embryos with cells of equal sizes and no fragmentation are considered grade 1 or the best quality. Some laboratories label embryos as:
- G (good) — all cells are equal size
- F (fair) — a few of the cells are different sizes
- P (poor) — cells are mostly all different sizes
An embryo with label 8AG will be considered the best. However, it must be noted that the symmetrical size of cells is not very significant in determining the quality the embryo or their growth potential.
Ideally, on Day 2 the embryo should have 4 cells and by Day 3, it should have 7-9 cells. According to some researchers (2), this cell number is perhaps the most important factor for determining the implantation potential of cleavage stage embryos.
It was also found (3) that faster growing embryos (those with higher number of cells on Day 3) has relatively lower implantation rate. Embryos having more than 9 cells on Day 3 were likely to have chromosomal abnormalities (4).
Day 5 embryo grading
Blastocyst grading is mainly done using the Gardner system (Gardner and Schoolcraft 1999).
By day 5 as the embryo continues to grow, the number of cells increases and at this stage the cells also start to differentiate into specific cell types. By this time, the outer covering (ZP) becomes thinner, so the blastocyst can burst through it an implant into the uterine lining.
The day 5 embryo (or blastocyst) has 2 kinds of cells:
- Inner cell mass (ICM), which will eventually form the fetus
- Trophectoderm Epithelium (TE), which will form tissues needed during pregnancy (like the placenta)
A blastocyst is like a fluid-filled sac with the TE cells on the outside and the ICM on the inside.
Both of these cell types are essential for a healthy pregnancy as they form the fetus and the placenta.
So, blastocyst grading involves assigning a separate letter grade to each cell type as well as to the cell cavity or blastocoel, which is filled with fluid. The size of the embryo and the number of cells in it are also noted at this point.
The three parameters of embryo grading on Day 5
Number: Based on the expansion of blastocyst
The expansion of a blastocyst gives an indication of its ability to develop and grow. An embryo that does not expand, will not be able to grow.
| 1 | Early blastocyst | Blastocoel or the cavity comprises less than 50% of the volume of the embryo |
| 2 | Blastocyst | Cavity takes more than half the volume of the embryo |
| 3 | Expanding | The outer membrane has thinned and the cavity is fully expanded |
| 4 | Hatching | The embryo has expanded and is starting to burst through the ZP |
| 5 | Completely hatched | The embryo has burst out of the ZP |
First letter: Grade of the inner cell mass (ICM), which will form the fetus
| A | Well-defined, cohesive layer of many cells |
| B | Cells are loosely packed; may have a grainy appearance |
| C | Few large, dark cells that seem degenerative |
Second letter: Grade of the trophectoderm (TE), which forms the placenta and other supporting cells
| A | Many equal-sized, tightly packed cells that give a neat appearance |
| B | Irregular, loose layer of cells |
| C | Few cells placed very irregularly; maybe dark or grainy |
In a very early blastocyst, the cavity is just starting to form and the cells cannot yet be differentiated into the two types. An expanded blastocyst has a well-defined cavity, around 100-125 cells all covered with a thin ZP. The hatched blastocyst has over 150 cells with the embryo bursting out of the shell.
Embryo grading and IVF success rates
Embryo classification is not an absolutely accurate science, but it does give an indication of the possibility of its survival.
Well-developed blastocysts with healthy contents are obviously better for successful pregnancies. According to this study(5), higher graded blastocysts (e.g. 3AA) were found to result in higher pregnancy rates at around 65%. Blastocysts that were graded average (like 2AB, 2BA, 4AC) had about 50% pregnancy rates and poor quality blastocysts (such as 4CC, 2BB, 3BC, 4CB) resulted in pregnancy rates of only 33%.
However, there’s nothing like best embryo grading for transfer as we cannot determine the exact usability of an embryo simply by looking at a grading chart.
An embryo with 1CA grade might seem poor at first, but it may still be developing and might turn into grade 4AA within a day.
So, if you have frozen a few embryos of quality say 4AA, 4CB and 5BC and the best quality one doesn’t result in a live birth, it doesn’t mean all hope is lost. The other embryos may still result in a positive pregnancy and a healthy baby.
While it is helpful to know about your embryos’ grading, you should not be too disappointed if there are few seemingly-good embryos.
Infact, researchers(6) are now looking into other factors such as metabolomics that could impact the quality of an embryo.
IVF success with C grade embryos
It might be surprising that even though C grade embryos are normally not preferred for transfer, there is growing evidence that these embryos may actually result in positive outcomes:
Research published in the Journal of Reproductive Biomedicine Online (7), found that live birth rates with embryos given C grade were 34.6% as compared to 39% for grade B and 46.8% for grade A. The average age of women in this study was 30 to 32 and it was founded that the seemingly poorer embryos did not cause any increase in miscarriage.
So, you cannot decide the absolute fate of an embryo simply based on the way it looks.
Do embryo grades matter?
According to new research (8), only one- third of implantation failures can be attributed to the embryo quality while, other factors such as poor endometrial receptivity, or inadequate interaction of embryo–endometrial lining.
The importance and usability of embryo grading cannot be denied but your individual factors such as age, health, and the particular causes of infertility should all be considered in determining the possibility of IVF success.
Embryo morphology grading is a standard tool used by fertility specialists and embryologists around the world to select which embryos to transfer for the best outcomes.
References
- Racowsky, C., Stern, J. E., Gibbons, W. E., Behr, B., Pomeroy, K. O., & Biggers, J. D. (2011). National collection of embryo morphology data into Society for Assisted Reproductive Technology Clinic Outcomes Reporting System: associations among day 3 cell number, fragmentation and blastomere asymmetry, and live birth rate. Fertility and sterility, 95(6), 1985–1989. https://doi.org/10.1016/j.fertnstert.2011.02.009
- Rienzi, Laura et al. Significance of morphological attributes of the early embryo. Reproductive BioMedicine Online, Volume 10, Issue 5, 669 – 681 DOI: https://doi.org/10.1016/S1472-6483(10)61676-8
- J. Holte, L. Berglund, K. Milton, C. Garello, G. Gennarelli, A. Revelli, T. Bergh, Construction of an evidence-based integrated morphology cleavage embryo score for implantation potential of embryos scored and transferred on day 2 after oocyte retrieval, Human Reproduction, Volume 22, Issue 2, Feb 2007, Pages 548–557, https://doi.org/10.1093/humrep/del403
- Kroener, Lindsay L. et al. Increased blastomere number in cleavage-stage embryos is associated with higher aneuploidy. Fertility and Sterility, Volume 103, Issue 3, 694 – 698 DOI: https://doi.org/10.1016/j.fertnstert.2014.12.090
- Zhao, Y. Y., Yu, Y., & Zhang, X. W. (2018). Overall Blastocyst Quality, Trophectoderm Grade, and Inner Cell Mass Grade Predict Pregnancy Outcome in Euploid Blastocyst Transfer Cycles. Chinese medical journal, 131(11), 1261–1267. https://doi.org/10.4103/0366-6999.232808
- Bromer, J. G., & Seli, E. (2008). Assessment of embryo viability in assisted reproductive technology: shortcomings of current approaches and the emerging role of metabolomics. Current opinion in obstetrics & gynecology, 20(3), 234–241. https://doi.org/10.1097/GCO.0b013e3282fe723d
- Bouillon, Céline et al. Obstetric and perinatal outcomes of singletons after single blastocyst transfer: is there any difference according to blastocyst morphology? Reproductive BioMedicine Online, Volume 35, Issue 2, 197 – 207 DOI: https://doi.org/10.1016/j.rbmo.2017.04.009
- Craciunas, Laurentiu & Gallos, Ioannis & Chu, Justin & Bourne, Thomas & Quenby, Siobhan & Brosens, Jan & Coomarasamy, Arri. (2019). Conventional and modern markers of endometrial receptivity: a systematic review and meta-analysis. Human reproduction update. 25. 10.1093/humupd/dmy044. DOI: 10.1093/humupd/dmy044
Reviewd by: Dr. Meenakshi, PhD